ORAL DEVICE THERAPY FOR OBSTRUCTIVE SLEEP APNEA
ABSTRACT
The objective of this review is to highlight recent developments in oral devices (ODs) as an alternative to continuous positive airway pressure (CPAP) for Obstructive Sleep Apnea (OSA) treatment. OSA is a common sleep disorder characterized by recurring collapse of the upper airway during sleep, resulting in sleep fragmentation and oxygen desaturation. The role of dentistry in sleep disorders is becoming more significant, especially in co-managing patients with simple snoring and mild to moderate obstructive sleep apnea (OSA). The practicing dental professional has the opportunity to assist patients at a variety of levels, starting with the recognition of a sleep-related disorder, referring them to a physician for evaluation, and assisting in the management of sleep disorders. Almost every discipline in dentistry needs to be aware of sleep disorders and their potential impact. The American Academy of Sleep Medicine (AAOSM) has recommended (ODs) for use in patients with primary snoring and mild to moderate OSA. The category of mandibular repositioning or advancement devices (MRD/ MAD) is by far the most common type of ODs in use today. It protrudes the mandible forward, thus preventing or minimizing upper airway collapse during sleep.
Key Words: Obstructive sleep apnea, continuous positive airway pressure, The American Academy of Sleep Medicine, mandibular advancement devices.
INTRODUCTION
Sleep disordered breathing (SDB) is a collective term which includes simple snoring, upper airway resistance syndrome (UARS), and sleep apnea. Patients present with various symptoms, although almost all complain of snoring, witnessed breathing pauses, and excessive day time sleepiness.1 Sleep apnea is probably the most prevalent of all the sleep disorders and is classified as central, obstructive, or mixed; it may be mild, moderate, or severe. OSA is the most prevalent of all the apneas and the second most diagnosed respiratory condition after asthma.2 It is characterized by the occurrence of 5 or more episodes of complete (apnea) or partial (hypopnea) upper airway obstruction per hour of sleep (apnea-hypopnea index [AHI]) and is estimated to occur in around 24% of middle aged men and 9% of women.3 Classifications are determined as: Mild OSA: 5-15 episodes per hour, Moderate OSA: 16-30 episodes per hour, Severe OSA: in excess of 30 disturbances occur per hour of sleep. Daytime symptoms such as excessive sleepiness, cognitive impairment, and reduced quality of life require appropriate treatment. Furthermore the association of OSA with increased risk of motor vehicle accidents, cardiovascular morbidity, and all-cause mortality emphasize the need for effective long-term treatment.3-4 Although nasal CPAP provides the most reliable therapeutic modality and is the most widely used method to treat sleep disordered breathing today, it is also the most cumbersome one, patient acceptance, tolerance, and adherence is often low, thereby reducing effectiveness. Therefore, there is a major need for effective alternative treatments.5 Oral devices (ODs) are designed to improve upper airway configuration and prevent collapse through alteration of jaw and tongue position. Current practice parameters of the American Academy of Sleep Medicine (AASM) indicate (MAD) as a first-line therapy in patients with mild-to-moderate OSA and in more severe OSA patients who fail treatment attempts with CPAP therapy.5-6
PREDISPOSING FACTORS
OSA is now recognized not only as SDB but also as a syndrome involving multiple organs that increases the risks of heart failure, stroke, and cardiovascular-related mortality; moreover, it is causally related to hypertension.4 Obesity is the most important reversible risk factor for OSA.7 In non obese patients, craniofacial anomalies like micrognathia and retrognathia may also predispose to OSA. Orofacial features that may predispose to OSA include enlarged palatine tonsils, enlarged uvula, high-arched palate, nasal septal deviation, longer anterior facial height, steeper and shorter anterior cranial base, inferiorly displaced hyoid bone,disproportionately large tongue, a long soft palate, and decreased posterior airway space. In addition to obesity, age, ethnic background, genetic, and gender predilection, habits like consumption of alcohol, smoking, and sedatives may aggravate existing OSA. Alcohol relaxes the airway muscles, making it more prone to obstruction.4-7-8 Anatomically, a block could occur as a result of excess fat or inflamed tissues in the upper airway. The presence of tumors could also lead to a pathological blockage, and environmental factors like allergies and infections can influence the response of the airway dilators and hence the size of the airway.
PATIENT EVALUATION
Patient evaluation prior to treatment requires a skilled multidisciplinary team. The Association of American Sleep Disorders has published guidelines about the appropriate use of OD therapy and defines the respective roles of the physician and the dentist in this type of care.10 The initial patient assessment, differential diagnosis of sleep complaints, and overnight diagnostic monitoring by the sleep specialist determine the indications for treatment. This physician determines the patient’s suitability for an oral appliance. The dentist can also identify a patient with symptoms of snoring and OSA and refer him/her for medical and sleep evaluation.
TREATMENT OPTIONS
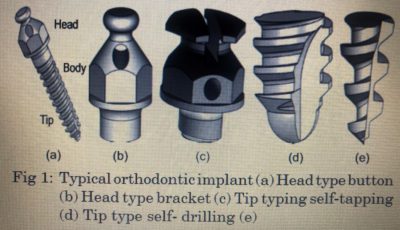
Treatment of sleep-disordered breathing (i.e. snoring, upper airway resistance syndrome, sleep apnea syndrome) can be divided into four general categories. These include: (1) lifestyle modification, i.e. weight loss, cessation of evening alcohol ingestion, sleep position training, (2) oral devices, (3) CPAP, and (4) upper airway surgery. The sleep medicine team defines possible treatment options for adult patients with OSA, based on the severity of the sleep disorder, preference of the patient, the patient’s general health, and the preference and experience of the team members. Less invasive treatment options are selected wherever possible. The first and simplest option is behavior modification; this would be followed by insertion of ODs suited to the patient, especially in those with mild to moderate OSA.2 The gold standard treatment for OSA is to pneumatically splint open the upper airway during sleep using continuous positive airway pressure CPAP. Although CPAP is highly efficacious in preventing upper airway collapse, patient acceptance, tolerance, and adherence is often low, thereby reducing effectiveness. Hence, there is a major need for effective alternative treatments. CPAP and surgical options are chosen for patients with moderate to severe OSA.2-5 ORAL DEVICES In 1991, The American Academy of Sleep Dentistry was formed for the education and certification of dental sleep-disorders specialists. In 1995, controlled studies indicated similar effectiveness of and greater patient preference for ODs compared with CPAP in mild to moderate OSA. In 2000, a section on oral appliances was created in the Academy of Sleep Medicine.11 Despite variations in OD design, the aim of all of these devices is to improve the patency of the upper airway during sleep by increasing its dimensions and reducing its collapsibility. ODs are basically thermoplastic materials with retainers and supports and are usually custom made. In broad terms, ODs can be categorized as: a. Mandibular repositioning or advancement devices (MRD/MAD) which may be titratable, e.g., Herbst appliance / snore guard / silencer. This category (MAD) is by far the most common type of ODs in use today. It protrudes the mandible forward, thus preventing or minimizing upper airway collapse during sleep. These devices can be either fixed (i.e. the protrusion distance cannot be changed), or variable (i.e. protrusion can be increased or decreased). The final protrusion distance represents a delicate balance between side effects and efficacy. A newly available remotely controlled mandibular titration device provides an objective mechanism by which to determine the maximal therapeutic level of mandibular protrusion during sleep. The amount of bite opening should be minimized to improve patient tolerance and increase the beneficial effect on upper airway dimensions.5-6 b. Tongue repositioning or retaining devices (TRD), can be used by edentulous patients, e.g., SnorEx.12 c. Soft-palate lifters.13 d. Tongue trainers.13 e. A combination of OD and CPAP in the new products delivers pressurized air directly into the oral cavity and eliminates the use of head gear or nasal mask and avoids the problems of air leaks and the claustrophobia associated with CPAP treatment.5-6-14
RATIONALE OF ORAL DEVICES
ODs are designed to improve upper airway configuration and prevent collapse through alteration of jaw and tongue position and this is the key mechanism by which treatment is delivered. The results show that upper airway obstruction during sleep may occur at any site between the nasopharynx and the larynx. The most common sites of obstruction are behind the base of the tongue (retroglossal) and behind the soft palate (retropalatal).14 ODs are worn only during sleep and work to enlarge the airway by moving the tongue (anteriorly) or the mandible to enlarge the airway. Whether they change the airway shape or increase the cross-sectional area of the upper airway is not clear. It is hypothesized that these devices may also affect upper airway muscle tone and thus decrease their collapsibility.6 Movement of the tongue or mandible anteriorly can increase the cross-sectional size of the airway and hence ODs help in increasing the airway size, although the increase in airway size may be the most important factor preventing airway occlusion.15 TRDs feature an extra-oral flexible bulb and hold the tongue forward by suction, preventing its collapse into the airway.5-6 A TRD is a custom-made soft acrylic appliance that covers the upper and lower teeth and has an anterior plastic bulb. It uses negative suction pressure to hold the tongue in a forward position inside the bulb. By holding the tongue in a forward direction through its attachment to the genial tubercle, it stabilizes the mandible and hyoid bone, thus preventing retrolapse of the tongue. These devices reverse pharyngeal obstruction both at the level of the oropharynx and the hypopharynx, thereby enlarging the airway and reducing snoring and the related apnea. Soft palate trainers and tongue posture trainers are rarely used. Newer ODs allow greater lateral jaw movement, cover all of the dentition, and provide better retention. Adjustable (titratable) devices allow the clinician to titrate the amount of mandibular protrusion in order to obtain an adequate treatment response. The selection of an appropriate design will vary on a case-by-case basis.5-16
EFFICACY
Treatment success is predominantly defined by a reduction in AHI with or without requirement for symptomatic improvement. Therapeutic success (designated as an apnea hypopnea index [AHI] of < 10 events per hour and a reduction in the AHI ≥ 50% from baseline).5-17 Comparison studies indicate that, compared to CPAP, ODs are less efficacious for improving the polysomnographic indexes of OSA. Despite this, there were similar improvements in subjective and objective measures of daytime sleepiness. In general, patients find ODs to be a more acceptable treatment compared to CPAP. It is common in clinical practice to continue mandibular advancement if residual apneas are seen and further protrusion is possible. Therefore, an even higher success rate may have been achieved.15 Cephalometric measurements such as increase in mandibular plane to cranial base angle are related to poor response to OD treatment, whereas shorter soft palate length, increased cranial base angulation, minimal retroglossal airway, short anterior face height, and mandibular retrusion have been related to successful OD treatment. These findings support the view that successful OD treatment is moderated by multiple anatomic factors. Recent studies utilizing magnetic resonance imaging, computed tomography, and cone-beam computed tomography have all provided valuable airway volumetric data that are not provided by two-dimensional cephalograms alone. Future research using volumetric airway imaging may provide valuable insights into predicting individual responses to OD therapy.2-15-17 ODs improve the blood oxygen saturation levels as they relieve apnea in 20-75% of patients. They reduce AHI to < 5 events per h in approximately 35 to 40% of patients and a partial response (≥ 50% reduction in AHI compared to baseline, but residual AHI remaining < 5 events per hour) in 25% of patients. Thus, approximately two thirds of patients can expect a clinically important response to ODs treatment.6 Mechanical variables that influence treatment efficacy and which may be adjusted in individual devices include jaw protrusion distance and angle of mouth opening. Efficacy may also affected by head and body posture during sleep. Most authors suggest that for adjustable MRDs, 50 to 75% maximal jaw protrusion maximizes efficacy without causing obvious TMJ problems. It has also been suggested that maximal jaw protrusion may increase the AHI.5 Evaluation of blood pressure of patients before and after treatment with oral devices could also indicate their efficacy. It is reported that after 4 weeks of MAD for OSAS patients with hypertension can lead to a significant fall of about by 3.5 mm Hg in awake blood pressure, associated with a reduction of AHI. This translates into reduction in the risk of stroke by 20% if this fall in blood pressure were maintained for two to three years.5-18 The fall in blood pressure with the use of oral devices was observed to be maximum in the early morning, which is the peak time for risk of myocardial infarction and stroke. A drop in the blood pressure at this time, it is suggested, will provide further protection against these adverse cardiovascular events.18-19 Most studies found in favor of a monobloc appliance (75% of maximum mandibular advancement) over treatment periods from 2 weeks to 3 months, a reduction in AHI and arousal index and improving oxygen saturation. Other studies also confirm OSA improvement specific to the MAD with reduction in AHI and improvement in arousal index, oxygen saturation, and REM sleep time. Reduced snoring and objectively measured sleepiness by the multiple sleep latency test (MSLT) were also found to be specifically related to the action of mandibular advancement.5 In adults with predominately moderate to severe OSA, the short term (one month) use of an adjustable MAD was not inferior to CPAP in its impact on 24 hour mean ambulatory blood pressure, daytime sleepiness, disease specific and general quality of life.19 The main advantages of using ODs are that there is good patient compliance and the devices are noninvasive and relatively inexpensive; they can also be easily carried anywhere by the patient.
FUTURE STUDIES
Recent advances in technologies related to MRD treatment have the potential to further improve their efficacy and effectiveness in clinical practice. The now commercially available remotely controlled mandibular
and positioner offers a means to predict response from a single-night mandibular titration study and has shown good positive predictive value in initial testing. The advent of new adherence monitoring technology that can be routinely incorporated into MRDs to objectively monitor treatment usage represents another advance in OSA treatment, which will be beneficial in practice and research. This will further help clarify the role of MRD in OSA treatment next to CPAP.2-5-17 In recent years, mandibular distraction osteogenesis has become the treatment of choice for pediatric patients with OSA that are associated with hypoplastic mandible.20
CONCLUSION
Although continuous positive airway pressure (CPAP) is the most efficacious treatment, it requires the use of a mask interface, sealed tubing, and a device connected to a power source tubing. This complexity limits its acceptance by patients and leads to suboptimal treatment adherence.15 Overall, ODs provide effective treatment for approximately two thirds of patients. ODs used to date constitute a relatively heterogeneous group of devices for the treatment of sleep apnea and non-apneic snoring. The evidence available at present indicates that ODS successfully “cure” mild-to-moderate sleep apnea in 40-50% of patients, and significantly improve it in additional 10-20%. They reduce, but do not eliminate snoring.6 Recent studies do not point to a clinically relevant difference between MAD and CPAP in the treatment of mild to moderate OSA.5-16 OD therapy should be carried out by a dentist with expertise in this field who is familiar with different types of appliances and can select the most appropriate one for the particular patient. There is no “best” appliance. The best one is that which is comfortable to the patient and achieves the desired efficacy. Side effects are common, but are relatively minor. Provided that the appliances are constructed by qualified dentists, 50–70% of patients continue to use them for several years. Their effectiveness is inferior to CPAP. It is similar to surgical procedures, but these are invasive, (although not particularly dangerous) and irreversible.5-7 There is a marked variability of individual responses to oral appliance therapy, and therefore the necessity to approach each patient on an individual basis.
REFERENCES
1 Schlosshan D, Elliott MW, Clinical presentation and diagnosis of the obstructive sleep apnoea hypopnoea syndrome, Thorax 2004; 59: 347-52.
2 Weaver TE, Calik MW, Farabi SS, Fink AM, Galang-Boquiren MT. et al., Innovative treatments for adults with obstructive sleep apnea, Nature and Science of Sleep 2014; 6: 137-47.
3 Sutherland K, Vanderveken OM, Tsuda H, Marklund M, Gagnadoux F. et al., Oral Appliance Treatment for Obstructive Sleep Apnea: An Update, J Clin Sleep Med 2014; 10(2): 215-27.
4 Ayas N, Skomro R, Blackman A, Curren K, Fitzpatrick M. et al., Obstructive sleep apnea and driving: A Canadian Thoracic Society and Canadian Sleep Society position paper, Can Respir J 2014; 21(2): 114-23.
5 Yu Q, Yin G, Zhang P, Song Z, Chen Y. et al., Distinct Associations between Hypertension and Obstructive Sleep Apnea in Male and Female Patients, PLoS ONE 2014; 9(11): e113076.
6 Chan AS, Lee RW and Cistulli PA. Dental Appliance Treatment for Obstructive Sleep Apnea, CHEST 2007; 132: 693-99.
7 Trakada G, Chrousos G, Pejovic S, and Vgontzas A. Sleep Apnea and its association with the Stress System, Inflammation, Insulin Resistance and Visceral Obesity, Sleep Med Clin. 2007 June; 2(2): 251-61.
8 Kang HH, Kang JY, Ha JH, Lee J and Kim SK. et al., The Associations between Anthropometric Indices and Obstructive Sleep Apnea in a Korean Population, PLoS ONE 2014;
9(12): e114463. 9 Zhu SJ, Wang QY, Zhou SH, Bao YY, Wang SQ. Obstructive sleep apnea syndrome caused by uncommon tumors of the upper aerodigestive tract, Int J Clin Exp Pathol 2014; 7(10): 6686-93.
10 American Sleep Disorders Association. Practice Parameters for the Treatment of Snoring and Obstructive Sleep Apnea with Oral Appliances, Sleep 1995; 18: 511-3.
11 Ivanhoe JR, Attanasio R. Sleep Disorders and Oral Devices, Dent Clin North Am 2001; 45: 733-58.
12 Schonhofer B, Stoohs RA, Rager H, Wenzel M, Wenzel G, Kohler D. A new Tongue Advancement Technique for Sleep -Disordered Breathing: Side effects and Efficacy, Am J Respir Crit Care Med 1997; 155: 732-8.
13 Schlosshan D, Elliott MW. Sleep, part 3: Clinical Presentation and Diagnosis of the Obstructive Sleep Apnoea Hypopnoea Syndrome, Thorax 2004; 59: 347-52.
14 Andrew Ng, Gotsopoulos H, Darendeliler AM and Cistulli PA. Oral Appliance Therapy for Obstructive Sleep Apnea, Treat Respir Med 2005; 4 (6): 409-22.
15 Almeida FR, Mulgrew A, Ayas N, Tsuda H, Lowe AA, Fox N, Harrison S, Fleetham JH. Mandibular Advancement splint as short-term Alternative treatment in Patients with obstructive sleep Apnea Already effectively treated with Continuous Positive Airway Pressure, Journal of Clinical Sleep Medicine 2013; Vol. 9: No. 4.
16 Aarab G, Lobbezoo F, Hamburger HL, Naeije M. Oral Appliance Therapy versus Nasal Continuous Positive Airway Pressure in Obstructive Sleep Apnea: A Randomized, Placebo-Controlled Trial, Respiration 2011; 81: 411-19.
17 Patrick J, Strollo Jr. Another Advance in Oral Appliance Therapy? Commentary on Remmers et al. Remotely controlled mandibular protrusion during sleep predicts therapeutic success with oral appliances in patients with obstructive sleep apnea, SLEEP 2013; 36: 1517-25.
18 Hoffstein V. Review of oral appliances for treatment of sleep-disordered breathing, Sleep Breath 2007; 11: 1-22.
19 White DP, Shafazand S. mandibular advancement Device vs Cpap in the treatment of obstructive Sleep apnea: are they equally effective in Short term Health outcomes? J Clin Sleep Med 2013; 9(9): 971-72.
20 Rachmiel A, Nseir S, Emodi O. Aizenbud D. External versus Internal Distraction Devices in Treatment of Obstructive Sleep Apnea in Craniofacial Anomalies, Plast Reconstr Surg Glob Open 2014;2:e188; doi: 10.1097/GOX.0000000000000147; Published online 29 July 2014.